Of course it can. But, we wouldn’t be doing us, you as pet owners, or the pets in your care any justice if we didn’t go into a little more detail. Here at My Pet Nutritionist we’ve seen hundreds of pets with joint concerns. Prevention is better than cure and this is where nutrition can certainly play a role. Even in chronic degeneration, there are changes that can be made for the better. Sadly, there are genetic dispositions to joint issues, and we can’t change that, but we can do a little bit of damage limitation.
There’s certainly a lot to cover, so let’s get cracking.
The Skeleton
The Skeleton is essentially a supporting framework. It consists of strong, mineralised bone which form a sophisticated system to facilitate movement.
Bone is a light, yet strong connective tissue consisting of around 30% collagen and other matrix proteins with around 70% minerals. These minerals include calcium and phosphorus, but magnesium, sodium and potassium are also present in conjugated form.
Bones come together to form joints. The type of joint formed determines the degree and direction of motion. For example, joints with a ball and socket formation allow for a rotation whilst hinge joints only allow for bending and straightening. In a joint, the ends of the bones are covered in cartilage, which helps reduce friction as joints move. With age, this cartilage can degrade. Tendons connect muscle to bone and are made up mostly of collagen. Ligaments surround joints and help to stabilise them. They also connect bone to bone.
Bone Formation
Also known as ossification, bone formation is a process where new bone is produced. Bone starts as a cartilage model which gets slowly replaced. Osteoblasts are the cells that form new bone; think of it as a blast that spreads, and osteoblasts spread to form new bone. Osteoblasts secrete osteoids which are simply unmineralized bone tissue. Soon after the osteoid is laid down, inorganic salts (calcium and phosphorus) are deposited which forms the hardened material that we know as bone.
Inappropriate levels of calcium and phosphorus during growth therefore understandably contribute to bone deformities and skeletal disorders. Diets high in phosphorus, particularly with low calcium reduce bone mass and density. We see this in the, now thankfully rare, disease in horses. Big head disease, more common in countries like Australia, is also known as bran disease or Miller’s disease.
The colloquial names demonstrate immediately the dietary link. Clinically termed hyperparathyroidism, it affects the skeleton of horses. The horse’s bones slowly demineralise due to the low levels of calcium found in their system.
The low calcium levels are usually due to one of two reasons.
Calcium bioavailability due to high levels of phytates in bran,
Calcium bioavailability due to oxalate containing grasses.
As we know, phytate is when phytic acid binds to a mineral. Phytic acid is the principal storage form of phosphorus, and it binds to zinc, iron, calcium, magnesium and more! What this means is that the mineral it binds to is less available. Sadly, phytic acid is found in plant-foods like grains, nuts and legumes and for us pet owners, of note, it is found in wheat, barley, rice and maize; the same ingredients found in many commercial pet foods. There is therefore the possibility that phytate can affect calcium bioavailability and be of detriment to bone formation, growth, and maintenance.
Oxalic acid is an organic compound found in many plants including leafy greens, vegetables, fruits, nuts and seeds. This too can bind to minerals including calcium and then becomes calcium oxalate. This not only results in low calcium levels, of detriment to bone formation, growth and maintenance but
may also lead to renal issues and/or failure.
It seems however, that high phosphorus and high calcium diets blunt the effects of each other. These two minerals interact in the gastrointestinal tract to limit absorption of the other. Therefore, a calcium: phosphorus ratio of 1.1:1 to 2:1 is recommended for dogs.
On the subject of the gastrointestinal tract, most minerals are absorbed largely in the small intestine (although they can be absorbed from any portion in the GI tract). So, the digestive tract needs to be working as it should to aid absorption and therefore utilisation of the minerals. Inflammation within the GI tract is often linked with vitamin and mineral deficiency.
Findings Here
Furthermore, those suffering with inflammatory bowel conditions are often treated with medications like glucocorticoids to reduce the inflammation caused by the disease. In the process, these medications disrupt the development and maintenance of healthy bones.
Bone formation proceeds outwards from ossification centres; short bones tend to have one in the middle whereas long bones typically have three, one at each end and one in the middle. Ossification, or bone formation continues until there is a thin strip of cartilage left at each end of the bone. This is known as the epiphyseal plate, or growth plate in the dog world. When the bone reaches full adult maturity, the cartilage is replaced with bone and “sealed” for want of a better word.
Glucocorticoids have a direct, inhibitory effect on the growth plate, as demonstrated by in vivo and organ culture studies. Glucocorticoids slow longitudinal bone growth by inhibiting chondrocyte proliferation, hypertrophy, and cartilage matrix synthesis. In vivo, dexmethasone, a potent synthetic glucocorticoid, infused directly into the proximal tibial growth plates of young rabbits caused a 77% inhibition in growth.
Findings Here
It would therefore be appropriate to consider the root cause of any inflammatory conditions alongside any treatment plan.
When considering calcium and phosphorus absorption, it pays to consider vitamin D because it stimulates the intestinal absorption of those minerals. Vitamin D is a fat-soluble vitamin found in foods like oily fish, liver, and eggs.
Being a known contributor to bone health, when puppies are fed a diet lacking in Vitamin D, they can develop Rickets. However, at the other end of the scale, puppies fed too much vitamin D experience impaired ossification (bone formation).
Findings Here
Sadly, there are several mechanisms which reduce the absorption, production, and activity of Vitamin D.
GI Issues
Vitamin D is absorbed in the small intestine. It is then converted in the liver and kidneys into a usable form. Interestingly there is a history of Vitamin D deficiency in the onset and activity of irritable bowel syndrome. Deficiency is also present in cases of Ulcerative Colitis.
Findings Here
Obesity
Vitamin D deficiency is often associated with obesity, despite there being much debate on the reasons behind it. What is important; there is a categoric decrease in bioavailability of Vitamin D in obese individuals.
Findings Here
Low-fat diets
Vitamin D is a fat-soluble vitamin, meaning it requires fat to be absorbed. Those on low-fat diets or with conditions that impair fat absorption (like IBS, IBD or liver issues) are more likely to have low Vitamin D levels.
Findings Here
In cases of pancreatitis, a low-fat diet is often recommended without consideration of the knock-on effect on other key nutrients. Again, it pays to consider the treatment plan of existing conditions in light of the effect they have on nutrient absorption.
Liver Disease
Foods to Feed in Liver Disease
Pancreatitis: Natural Guide for Pets
There are a range of medications that can impair the absorption of vitamin D including antibiotics, anti-inflammatory agents, endocrine drugs, and herbal medicines like St. John’s Wort. It is thought that through the medication action on certain receptors in the body, there is increased degradation of the active form of vitamin D. Whilst there is a place for many of these medications in certain cases, information is power, and adjustments may be necessary to ensure your pet is gaining the nutrients they need for health.
Despite us knowing it as the sunshine vitamin, dogs don’t have the same capacity to produce vitamin D from the sun, so they rely solely on dietary sources.
Joint Degradation
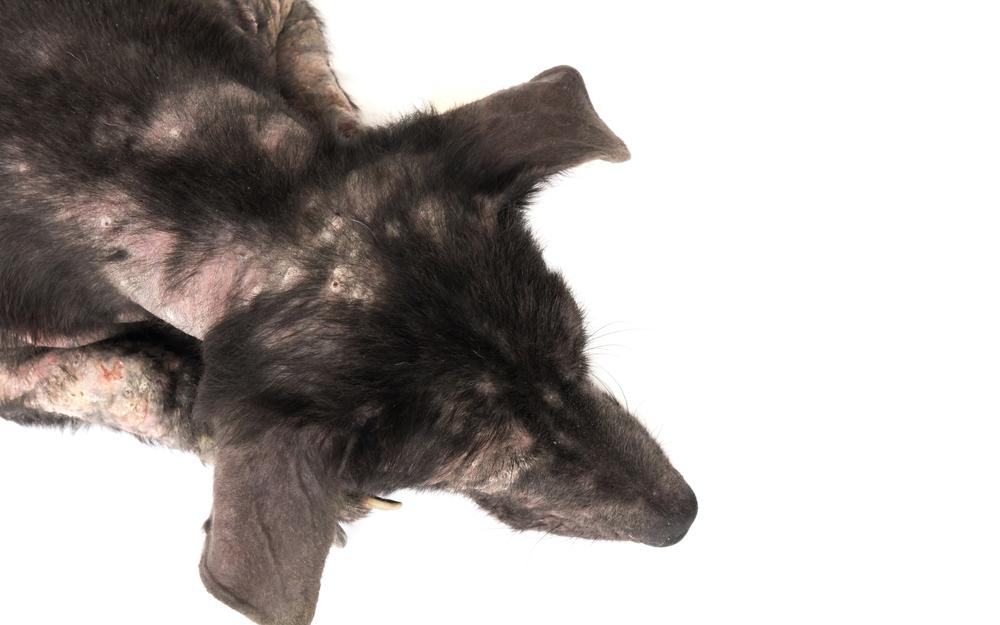
Joint degradation is characterised by inadequate production of compounds necessary to its structure, along with reduced collagen synthesis and it has a number of risk factors:
- Nutritional insufficiency
- Physical stress or trauma
- Overuse – aging
- Excess weight
- Autoimmunity
In these cases, inflammation is upregulated. It results in weak, damaged, or inflamed tissue with restricted or painful movement.
There is increasing consideration that gut dysbiosis is a major driver in inflammatory conditions. It is suggested that impaired digestion due to low stomach acid or enzyme production (pancreas or liver issues) could lead to increased dietary allergens permeating the gut wall, creating inflammatory responses throughout the body. So, alongside bone or joint issues, there may be a need for gut healing.
What Can Cause Gut Dysbiosis
What Can Help Gut Dysbiosis
Optimal Gut Health For Dogs
An imbalance of essential fatty acids may also predispose to pro-inflammatory compounds.
Eicosanoids are products of the oxidation of the omega families and they play an important role in the body. They modulate many processes including reproduction, blood pressure, haemostasis (the process to prevent and stop bleeding) and inflammation.
They can be synthesised from AA, GLA and EPA fatty acids, however, those synthesised from AA are proinflammatory compared to those derived from GLA and EPA and it is believed that those derived from AA in high amounts can result in disease.
Human studies have demonstrated that the supplementation of algae oil significantly alters the ratio of EPA (omega-3) to AA (omega-6) in cell membranes which has been beneficial in inflammatory conditions. A literature review of 20 studies into arthritis revealed that 16 of those demonstrated an improvement after omega-3 supplementation.
Essential Fats For My Dog
Inflammatory processes also induce oxidative stress and reduces cellular antioxidant capacity. Overproduced free radicals react with cell membrane fatty acids and proteins impairing their function permanently. Oxidative stress is the imbalance between free radicals and antioxidants, and so when tackling any inflammatory condition, it is essential to consume sufficient antioxidants.
External sources of oxidative stress like air pollution, rancid fats, foods cooked to high temperature, toxin exposure and many more will further increase the burden, so it’s important to limit exposure to these too!
Top Tips for Joint Health
- A fresh food diet rich in absorbable nutrients
- Provide foods containing key vitamins and minerals (calcium, phosphorus and vitamin D for example)
- Offer essential fatty acids (omega 3)
- Ensure digestive health (undertake gut healing if necessary)
- Limit oxidative stress
We also have a number of additional blogs specifically relating to joint health, find them here:
Natural Arthritis Guide
How To Choose a Good Joint Supplement
Groovy Green Lipped Mussels for Joints
As you have likely gathered, nutrition is such a small piece of the puzzle when considering joint health. If you would like support with your pet’s health, then please check out our services.
Thanks for reading,
MPN Team x