Here at My Pet Nutritionist, we are often presented with a range of tests, that seemingly identify what your pet is allergic to. These tests will often even highlight how severe the allergy is.
But do you want to know a secret?
They often don’t help.
We realise that this may a bold statement, so we’ll explore the mechanism behind allergies in a little more detail, and why there are better tools to establish what’s going on in your pet.
An allergy is an unnecessary immune response to an innocuous substance, but a true allergy can be fatal.
Immune Responses
The innate immune system provides the first line of defence; broadly divided into physical/chemical barriers and nonspecific response.
The physical barriers include the skin and mucosa of the digestive and respiratory tracts. Saliva, tears, and mucous all help to provide a barrier, as does the microbiome of the skin and gut and of course stomach acid. Hair inside the nasal capacity also traps pathogens and environmental pollutants.
Pathogens that sneakily get past these first defences are next welcomed by the nonspecific innate response.
Here cells recognise and bind to pathogens and engulf them. White blood cells are recruited to the site of infection, leading to the well-known inflammatory response.
The inflammatory response, whilst often on the receiving end of bad press, is a vital response to injury, infection,trauma, and other insults. Mast cells release histamine, and histamine causes blood vessels to widen, there by increasing blood flow to the area and so, we have the usual signs like redness, heat, swelling and pain associated with inflammation.
Mast cells are particularly numerous at potential sites of injury like the nose, mouth, feet, internal body surfaces and blood vessels. Histamine is also stored and released from cells in the stomach. Histamine is involved in stomach acid secretion, but it also has effects on smooth muscle which is why it is thought to be involved in increased peristalsis (movement of food through the digestive system) in food allergies. This is why antihistamine use can be implicated in poor digestive function.
The inflammatory response is also a key player in the third line of defence, adaptive immunity.
This system is likewise activated by exposure to pathogens, but it uses an immunological memory to learn about the threat and adjust its response accordingly. The adaptive immune response is much slower to respond to threats and it relies on fewer types of cells to carry out its work.
Some of these cells manufacture immunoglobulins which are proteins that circulate in the blood stream and bind to antigens (allergens).
Immunoglobulins also known as antibodies, abbreviated as Ig, are involved in our dog’s systems when they fight off infections, but they are also involved in sensitivities or allergic reactions to things in the environment or food.
A
food allergy or other allergic response is caused by an IgE antibody reacting towards that allergen.
IgE binds to mast cells to promote histamine release.
IgA is an antibody that lives in mucous membranes, inside nasal cavities, and lungs. It helps to protect the respiratory tract as a first line of defence.
IgM is the first immunoglobulin that is encountered in an infection, or vaccines for the first time.
IgG is the work horse antibody; it is the soldier, the memory antibody. This is what gets drafted when your dog is exposed to something they have already figured out a response to.
Here in lies the problem – many allergy tests claim to test IgG. IgG is the memory antibody – so all this is really indicating is exposure.
Tests Available
Blood – this test is where a sample of blood is taken. It has been noted to measure total IgE antibodies found in the blood, but there are also specificIgE tests which measure the level of antibodies in response to particular allergens. Other blood tests measure IgG antibodies. There are many test providers to be found online – so what they measure is usually very individual.
Fur – these tests are usually carried out using bio resonance technology which measures the frequencies emitted from the hair sample. It is based on the idea that unhealthy cells or organs emit altered electromagnetic waves due to DNA damage.
Saliva – these tests generally measure IgM, IgA and IgG. It is thought that the same immunoglobulins that are generally found in the blood, are found in the saliva, but this way is less invasive.
That said, there are food sensitivities that are deemed non-IgE, meaning they don’t recruit IgE antibodies, which would suggest a blood test would be inconclusive, despite showing symptoms like vomiting, bloating and diarrhoea.
What the Data Shows:
- Testing often show positive results for apparently healthy dogs (not demonstrating any symptoms of discomfort). Findings here
- There are often no clear differences in positive reactions between allergic dogs and healthy dogs. Findings here
- There is no clear difference in total IgE and IgG before starting an elimination diet, and completing an elimination diet, despite there being symptomatic improvement when re-challenged. Findings here
- When comparing saliva and fur samples from healthy and allergic dogs, the distribution of positive and negative results was no different to that expected by random chance. This sample also include fake fur. Findings here
This doesn’t mean the reaction doesn’t occur – what this means is that that testing is inconclusive.
For that reason, elimination diets remain the gold standard for diagnosing adverse food reactions in dogs.
Findings here
A true allergy can be fatal, but true allergies are less common than you would think.
In our pets, we are generally tackling sensitivities, and this often starts with a poorly functioning digestive system.
In normal conditions, the digestive tract should be impermeable to antigens. When it is damaged, antigens can boldly go where no antigen has gone before, resulting in the immune response we discussed earlier. The inflammatory response, if prolonged, can result in further damage, permeating other antigens, and so the cycle continues.
Therefore, gut healing is so important when tackling potential sensitivities along with modulating inflammatory responses.
Ultimately, when we are looking to support the gut, we follow the 4 R’s.
Remove – carry out an elimination diet. Remove offending foods, one at a time and note changes in symptoms. Quite often, even offending foods can be reintroduced at a later stage. Check out our article on elimination diets
here.
Repair – support immunity and gut healing with ingredients like slippery elm, de-glycerised liquorice, glutamine, andN-acetyl-glucosamine. It is also important to consider how existing medications are affecting gut healing for example, steroid use impairs intestinal absorption which is linked to several gastrointestinal dysfunctions. But,because of their anti-inflammatory and immunosuppressive activities, they are often prescribed in cases of allergies or intolerance.
Findings here
Restore – as the microbiome is key in the development of the immune system, supporting this is essential, however, the introduction of specific pre and probiotic foods or supplements is sometimes best left for a few weeks into your plan.
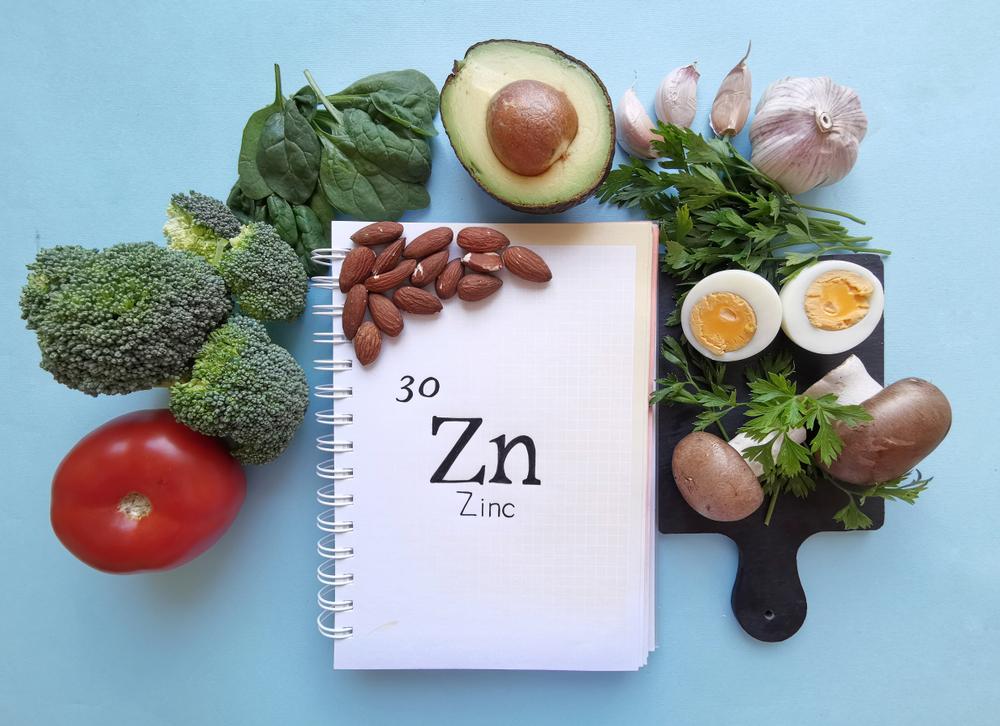
Replenish – indigestibility of food proteins can also contribute to their antigenic nature, so consider any long-term medication use include proton pump inhibitors which affect gastric acid secretion. Ensuring HCL, pepsin and digestive enzymes are in good supply will help get the digestive system back to doing what it does best!
It must also be remembered that there are certain genes which can result in immune system dysregulation or aberrant response. If you’d like to learn more about how a dysfunctional gene in the skin has been linked to secondary allergic disease, take a look at our blog
here.
The Bottom Line
Allergy or intolerance tests are often inconclusive and no matter where you look, elimination diets are still the gold standard for assessing adverse food reactions in dogs (and humans for that matter).
Tackling allergies or sensitivities can cause worry, fear, and anxiety. If you are then presented with a test result slip that, in short, suggests your dog can’t eat 85 out of the 90 foods tested, where do you go from there?
Well, here at My Pet Nutritionist, we take a step back. We look at the symptoms your dog is experiencing with a full history and we create a plan.
We don’t have a magic wand, but we do have many years’ experience tackling these issues.
If you’d like more information about the function of the immune system is its entirety, then check out our blog
here.
If you’d like to get to grips with the digestive system, take a look
here.
Finally, we have 7 of our top tips to optimal gut health
here.
But, if you would like to find light at the end of the tunnel, and not to realise it’s an oncoming train, we’d love to be apart of your healing journey.
Check out our services
here.
Thanks for reading!
MPN Team x