An elimination diet – the wand of all wands. Or at least we would like to think so. Here at
My Pet Nutritionist, we regularly utilise elimination diets in our healing plans. But there is often some confusion over their purpose and how best to use them.
So, we thought we’d cover, what they are, what they hope to do, and what they can’t do.
What is an elimination diet?
An elimination diet, also known as exclusion diet, is a diagnostic procedure used to identify foods that an individual/animal cannot consume without adverse effects. Adverse effects may be due to food allergy (IGE), food intolerance (IGG), other physiological mechanisms, or a combination of all of the above.
The point to note here is that it is a diagnostic tool – not a long-term lifestyle and in some cases, a means to give the immune system a welcomed break.
People often look at certain foods being the culprit or the saviour. But what’s really happening is the bodies inability to deal with certain antigens effectively.
As we know, the immune system functions like a radar – always on the lookout for potentially harmful compounds. But, through regular activation it can become hypersensitive and seemingly forget that it does have a tolerance capacity too.
Immune Tolerance
In the body, there are two types of immune tolerance, one is self-tolerance, and this prevents the development of autoimmune disease. The body accepts its own cells and doesn’t try to kill them (so kind!). But there is also this idea of induced tolerance.
Induced Tolerance
Induced tolerance occurs when the immune system actively avoids responding to an external antigen. This tolerance is induced by previous encounters with that antigen.
An example of induced tolerance is a deliberate manipulation of the immune system to avoid the rejection of transplanted organs or to provide protection from allergic reactions.
But induced immunity needs a fully functioning immune system to make the right calls at the right time – this is the basic premise of why we want to carry out an elimination diet. To see what foods might elicit a reaction.
Through the removal of antigenic compounds (the foods potentially wreaking havoc), you remove the adverse responses pulling on resources and you can then spend time supporting the various systems in the body, including the immune system, to get your ducks in a row.
Why would you do an elimination diet?
An elimination diet is often the first port of call for dogs suffering with allergies, intolerances, inflammatory conditions and also behavioural issues. This last point often raises a few eyebrows –but as we know, immune responses are intricately linked with the brain and subsequently behaviour.
We not only have sickness behaviour, which makes us hunker down and prevent the spread of virus (evolutionary purpose for survival), but pain simply makes us, and our dogs, miserable. In cases of irritable bowel syndrome, there is a noted visceral hypersensitivity too, which in a nutshell means an even higher sensitivity to pain (and sadly an increased propensity to be miserable).
The take home? Allergies, intolerances and inflammatory conditions are all an immune response. So, the point is to lighten the load on the immune system.
But we can’t forget there are differences between allergies and intolerances.
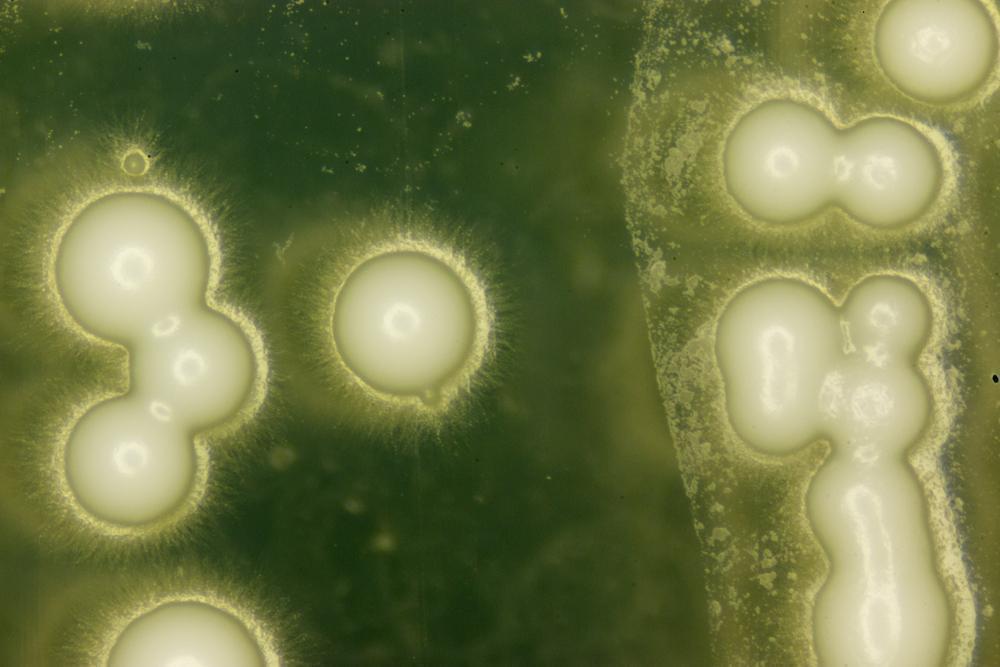
A food allergy or other allergic response is caused by an IgE antibody reacting towards that allergen. IgE binds to mast cells to promote histamine release. This is an immediate response and in some to certain food allergens can be fatal (anaphylaxis). Hives or instant rashes and swelling can be seen.
IgA is an antibody that lives in mucous membranes, inside nasal cavities, and lungs. It helps to protect the respiratory tract as a first line of defence.
IgM is the first immunoglobulin that is encountered in an infection, or vaccines for the first time.
IgG is the work horse antibody; it is the soldier, the memory antibody. This is what gets drafted when your dog is exposed to something they have already figured out a response to.
When you have a food intolerance, we tend to discuss it in terms of IgG. Symptoms usually begin within a few hours of eating the food that you are intolerant to. Yet, symptoms can be delayed by up to 48 hours and last for hours or even days, making the offending food especially difficult to pinpoint.
IgG’s are mostly raised from the barrier mucosa in the digestive system. After a meal, there are both antibodies and complexes of food antigens bound to specific IgG’s. These complexes are quickly cleared by the reticuloendothelial system.
Clinical observations suggest that due to gut inflammation and permeability (leaky gut), the digestive system is unable to digest the proteins effectively which subsequently raises IgG response to certain foods. We know that chronic intestinal inflammations and permeability are related to and possibly responsible for food IgG sensitivity.
90% of food reactivity comes from IgG’s. Just to confirm, intolerances can be changeable but allergies tend to be for life and only account for around 10% of food reactivity.
IgG’s come in different categories but to keep it simple, they are generally defined as cyclic or fixed. A common IgG reaction is cyclic and can take around 3 months to disappear/change. A fixed Intolerance tends to linger for longer and can take around 6 months to disappear/change.
So how do we move forward?
We prime and reset the digestive system, and this includes
starting with an elimination diet but also gut healing and immune balancing protocols.
We follow the 4 R’s.
–
Remove – carry out an elimination diet. Remove offending foods, one at a time and note changes in symptoms. Quite often, even offending foods can be reintroduced at a later stage.
–
Repair – support immunity and gut healing with ingredients like slippery elm, de-glycerised liquorice, glutamine, andN-acetyl-glucosamine. It is also important to consider how existing medications are affecting gut healing for example, steroid use impairs intestinal absorption which is linked to several gastrointestinal dysfunctions. But, because of their anti-inflammatory and immunosuppressive activities, they are often prescribed in cases of allergies or intolerance.
Findings here
–
Restore – as the microbiome is key in the development of the immune system, supporting this is essential, however, the introduction of specific pre and probiotic foods or supplements is sometimes best left for a few weeks into your plan.
–
Replenish – indigestibility of food proteins can also contribute to their antigenic nature, so consider any long-term medication use including proton pump inhibitors which affect gastric acid secretion. Ensuring HCL, pepsin and digestive enzymes are in good supply will help get the digestive system back to doing what it does best!
How do you carry out an elimination diet?
Raw or lightly cooked we’ve found is the best way to do this. Cooked foods can take pressure off the digestive system – which has often taken a bit of a beating in these cases.
Start with novel proteins (proteins your dog’s immune system has not seen before) –horse, ostrich, kangaroo and hare are generally well tolerated. Horse is lean too, so a great option if digestive function isn’t where it needs to be, yet.
Feed this novel protein for
4-12 weeks. Ideally if you land on a novel protein that helps the itch/digestive discomfort or doesn’t make it any worse, we recommend
remaining on this protein for 12 weeks -the time it takes for an intolerance to change.
Then introduce other novel proteins – but at no more than one per week and sticking to single source. Treats need to match too! No sneaky treats or chews.
If there are signs of intolerance, then remove that protein and go back to a protein you believe is best tolerated.
Notice that it’s called an elimination diet, and not an elimination lifestyle. The overall aim is to eventually maintain a strong diversity in the diet, as we know this supports optimum gut health. We would be looking to reintroduce more common proteins as time went on – but this takes time. We also practice the same process on reintroducing any fruit or vegetables – one at a time, over time. It can also be worthwhile opting for a low-histamine approach when reintroducing, check out our low histamine blog
here.
An Elimination Diet in a Nutshell
- To remove the burden on the immune system – by removing triggers
- Support immune and digestive function
- Support immune tolerance – some dogs eventually tolerate the original antigenic food once their system has their ducks in a row (note: this is for sensitivities and not in fact true allergies)
- Short term
- One tool (of many) for itchy dogs
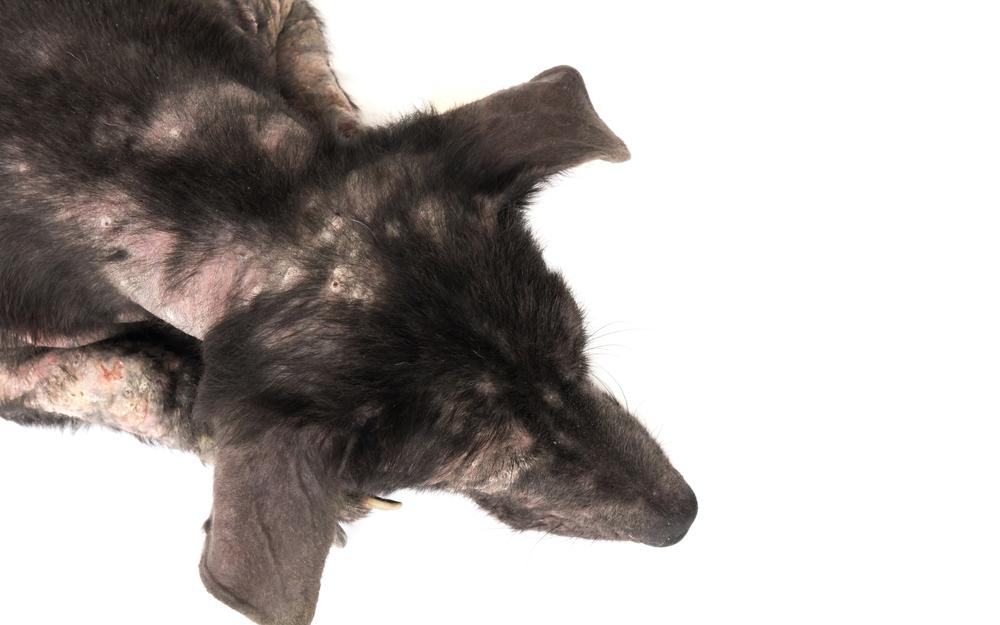
Environmental Antigens
The same premise also applies to environmental triggers – by removing triggers, you are reducing the load on the immune system. Quite often both food and the environment are intricately intertwined – when the burden is reduced in one area, symptoms in the other improve. Equally, if you are focussing on one area without consideration for the other, it can feel like you are banging your head up against a brick wall.
The bottom line – context matters. Which is why here at
My Pet Nutritionist we take a holistic view of the pet in front of us to establish possible root causes of the issues they are experiencing. The vast range of possible causes means we have grown our tool chest significantly over the years – but we still don’t have a magic wand.
An elimination diet is not a magic wand – but it is a place to start and one we have much experience in running alongside immune and detoxifying support.
We often get asked about intolerance and allergy testing and whether this is a helpful tool. We feel this deserves a blog of it’s own and will be coming next week.
If you would like our help to support your pet’s health, then please check out our services
here.
Thanks for reading!
MPN Team x